KLINICKÉ A VĚDECKÉ STUDIE
cerabone® je jedním z nejlépe zdokumentovaných materiálů pro augmentace kostí na celém světě.
Více než 150 studií dokazuje jedinečné vlastnosti materiálu
a klinickou účinnost cerabone® v regenerativní zubní medicíně.
cerabone® je v současné době předmětem více než 30 předklinických a klinických výzkumných projektů na globálních akademických institucích.
DLOUHODOBÝ ÚSPĚCH
Augmentace okolo zubních implantátů implantovaných do kosti pomocí bovinního materiálu cerabone®, nebo kombinace augmentace vlastních kostních štěpů a cerabone® prokázaly kumulativní míru přežití na 98.73 – 100%
průměrné sledování 12 – 65,93 měsíců po operaci 1-5.
MÍRA PŘEŽITÍ
98,73 – 100%
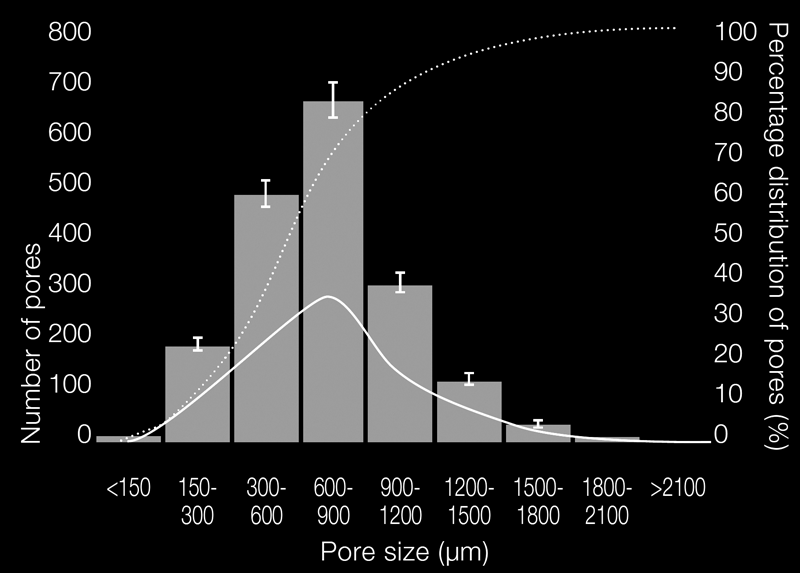
Snímky z elektronového mikroskopu (SEM) ukazují vysoce strukturovaný povrch cerabonu ®,
stejně tak jako makro- a mikropory.
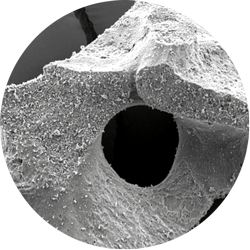
Makroporézní struktura umožňuje migraci buněk, penetraci krevních cév a integraci částic
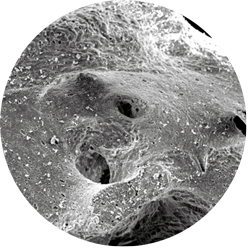
Kapilární účinek mikropórů umožňuje rychlou absorbci krve

Hrubý povrch zajišťuje vynikající a homogenní povrchovou adhezi buněk a proteinů
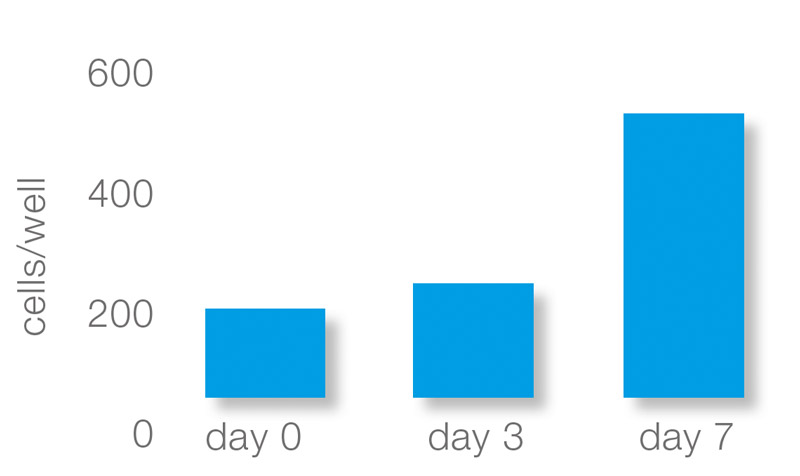
Růst osteoblastů a osteoklastů v cerabone®
in vitro výsledky od Prof. Dr. Dr. D. Rothamel, Clinic Mönchengladbach, University of Düsseldorf a PD Dr. C. Reichert, University of Bonn
Hrubý povrch také podporuje adhezi sérových proteinů a buněk k povrchu cerabone®. Buňky podobné osteoblastům rychle ulpívají na částicích cerabonu®. Pouze připojené osteoblasty mohou začít vytvářet novou kostní matrici, což vede k kostní integraci částic cerabone®. Další studie ukázala, že dobrá přilnavost osteoklastů podporuje povrchovou remodelaci částic.
VÝZKUM KMENOVÝCH BUNĚK
Interakce cerabone® s kmenovými buňkami
in vitro výsledky od prof. Dr. B. Zavana, University of Padova
cerabone® podporuje diferenciaci připojených kmenových buněk na osteoblasty, které produkují novou kostní matrici. Kolagen, osteopontin, osteonektin a osteokalcin jsou proteiny extracelulární kostní matrice, které lze použít jako markery pro tvorbu kostí. Jejich detekce 14 dní po aplikaci kmenových buněk na cerabone® naznačuje správnou diferenciaci buněk.
interakce cerabone® s lidskými kmenovými buňkami zubní dřeně
In vitro data od Khojasteh et al. 7
cerabone®; podporuje adhezi, proliferaci a diferenciaci lidských kmenových buněk zubní dřeně (hDPSC) nasazených na částice. Skenovací elektronové mikrofotografie (SEM) ukázaly, že hDPSC prokázaly fibroblastický fenotyp s několika cytoplazmatickými prodlouženími 14 dní po inkubaci na částicích cerabonu®.
VYBRANÉ PUBLIKACE
SINUS FLOOR AUGMENTATION
STUDY BONE GRAFT DISPLACEMENT AFTER MAXILLARY SINUS FLOOR AUGMENTATION WITH OR WITHOUT COVERING BARRIER MEMBRANE: A RETROSPECTIVE COMPUTED TOMOGRAPHIC IMAGE EVALUATION
Ohayon L, Taschieri S, Friedmann A, Del Fabbro M. Int J Oral Maxillofac Implants. 2019 May/June;34(3):681–691.
https://www.ncbi.nlm.nih.gov/pubmed/30521657
The goal of this retrospective study was to evaluate, if a collagen barrier membrane placed over the lateral bone window affects the stability of the bone graft and the displacement of bone graft particles following sinus floor augmentation.
Methods:
41 patients did underwent lateral sinus floor augmentation using cerabone®. The bone windows were either covered with collprotect® membrane (control group, n=17) or left uncovered (test group, n=24). All sites were closed by the flap. CBCTs were taken immediately after the surgery, and seven days as well as six months post-operative in order to evaluate bone graft stability and bone graft particle displacement. Post-surgical morbidity was analyzed using a visual analog scale (VAS) seven days after the surgical intervention.
Results:
– Mean displacement of the bone graft particles six months post-operative was significantly greater in the test group (3.8±3.1 mm) than in the control group (0.5±0.4 mm)
– Post-operative morbidity was significantly more pronounced in the test group (pain 3.3±1.4/swelling 4.3±4.5) than in the control group (2.1±0.9/2.7±0.9)
Conclusion:
The authors concluded that a barrier membrane placed over the lateral bone window helped preventing bone graft particles displacement thus reducing post-operative morbidity.
EXTRACTION SOCKET MANAGEMENT
STUDY PRESERVATION OF PERI-IMPLANT HARD TISSUES FOLLOWING IMMEDIATE POSTEXTRACTION IMPLANT PLACEMENT. PART I: RADIOLOGIC EVALUATION.
Cardaropoli D, Tamagnone L, Roffredo A, De Maria A, Gaveglio L. Int J Periodontics Restorative Dent. 2019 Sep/Oct;39(5):633-641.’
https://www.ncbi.nlm.nih.gov/pubmed/31449572
This study describes the immediate placement of dental implants in post extraction sockets for preservation of the alveolar ridge dimensions.
Methods:
20 patients requiring single tooth extractions were enrolled in the study. Following extraction, granulation tissue was removed and the implant bed was prepared. Before implant placement, a specifically designed bone plugger was inserted to accurately graft the peri-implant gaps using small cerabone® granules. The implant was installed, Emdogain® was applied on top of the graft and a provisional screw-retained abutment was placed. Finally, the definitive crown was delivered three months later. Marginal bone level (MBL) – and ridge width changes were evaluated using intraoral radiographs and CBCT images respectively, which were taken at implant placement (T0) and 12 months post-loading (T1).
Results:
– Uneventful healing at all treated sites
– Mean MBL was 2.70 ± 1.19 mm at T0 and 2.28 ± 1.34 mm at T1 (P < 0.05)
– Ridge width changes (T0 – T1) were as follows: 0.59 ± 0.47 mm at the crest, 0.49 ± 0.36 mm 3 mm below the crest and 0.43 ± 0.32 mm 6 mm below the crest
– Preservation of the horizontal ridge dimensions (T0 – T1) were accordingly: 93.18% ± 5.33% at the crest, 94.37% ± 4.41% 3 mm below the crest, 95.13% ± 3.66% 6 mm below the crest
– Ridge width changes were independent of the buccal plate thickness
Conclusion:
The authors concluded that immediate implant placement with immediate restoration supports the preservation of the alveolar ridge volume. Marginal bone level was demonstrated to be stable over the observation period of 12 months. An accurate grafting as presented with cerabone® of the peri-implant bone gaps was considered crucial to minimize marginal bone level changes.
STUDY PRESERVATION OF PERI-IMPLANT SOFT TISSUES FOLLOWING IMMEDIATE POSTEXTRACTION IMPLANT PLACEMENT. PART II: CLINICAL EVALUATION.
Cardaropoli D, Tamagnone L, Roffredo A, De Maria A, Gaveglio L. Int J Periodontics Restorative Dent. 2019 Nov/Dec;39(6):789-797.
https://www.ncbi.nlm.nih.gov/pubmed/31613939
The goal of the study was to evaluate marginal soft tissues changes of immediately placed and restored implants.
Methods:
Following single tooth extractions in the anterior maxilla, the sockets were debrided and the implant beds were drilled. Prior implant placement, the peri-implant gaps were grafted using small cerabone® granules. Emdogain® was applied on top of the graft after implant insertion and a provisional screw-retained abutment was placed. The definitive crown was delivered three months later. Mesial papillary level (MP), distal papillary level (DP) and midfacial gingival level (MG) were evaluated at implant placement (T0) and 12 months post-loading (T1) using a reference stent. In addition, a pink esthetic score (PES) was analysed.
Results:
– Uneventful healing at all treated sites
– 100% implant survival rate
– No statistical differences for MP, DP, MG and PES between T0 and T1 were found
– No statistical differences between thin and thick biotypes were found
Conclusion:
The authors concluded that immediate implant placement and restoration support the preservation of the marginal soft tissues. No correlation for the gingival biotype was found.
STUDY DIGITALIZED CAD/CAM PROTOCOL FOR THE FABRICATION OF CUSTOMIZED SEALING SOCKET HEALING ABUTMENTS IN IMMEDIATE IMPLANTS IN MOLAR SITES.
Finelle G, Sanz-Martín I, Knafo B, Figué M, Popelut A. Int J Comput Dent. 2019;22(2):187-204.
https://www.ncbi.nlm.nih.gov/pubmed/31134225
This case series aimed to evaluate the performance and efficacy of a digitally fabricated sealing socket abutment in implant immediacy.
Methods:
Molars in the mandible or maxilla were extracted atraumatically (patients n=29) and implants (n=30) were placed in the irrigated and cleaned sockets. Small cerabone® granules were placed around the implants to augment the gaps. A digital impression was taken and based on that a customized healing abutment was milled chairside. Then, the abutment was placed onto the implants. After three to four months, the abutment was removed and a digital impression was taken for preparation of the final prosthesis. The clinical outcomes were evaluated at one and two years post-surgery.
Results:
– Uneventful healing for all patients one week after abutment placement
– Maintenance of the buccal contours over the 2-year follow up period
– All implants remained successfully in situ over the 2-year follow up period
Conclusion:
The authors summarized that the use of a CAD/CAM-fabricated healing abutment in immediate implant placement is a viable treatment option for the management of molar extraction sites.
CASE REPORT IMMEDIATE PLACEMENT AND RESTORATION OF A NEW INNOVATIVE FULLY-TAPERED IMPLANT REPLACING CENTRAL AND LATERAL INCISORS
Dada K, Pariente L, Daas M, Montenero J. (2019) International Dentistry – African Edition Vol. 8, No. 6, p. 48 – 54.
http://www.moderndentistrymedia.com/dec_jan2019/dada.pdf
This case report describes the use and performance of a newly developed implant in immediate implant placement.
Methods:
Teeth 11 and 12 of a 52-year old patient were diagnosed hopeless and extracted consecutively. First, tooth 11 was extracted and an immediate implant placement procedure was performed using a Straumann® BLX Implant. Following implant insertion, a temporary abutment for the crown was installed and the gap between the implant and the buccal bone wall was augmented with cerabone® granulate. Finally, a screw-retained temporary crown was installed. Three months later tooth 12 was extracted and a socket preservation was performed using cerabone® and an autologous soft tissue punch. Two months following healing the final prosthetic restoration was done using a zirconia cantilevered implant supported bridge.
Results and Conclusion:
The gingival contours were well preserved ten months post-surgery. The authors appreciated the advantages of an immediate implant placement procedure, which are a reduced treatment time and less surgical interventions. The use of a volume stable bone graft were considered favorable in preserving the ridge dimensions. Installation of an implant supported provisional crown in the described procedure helped maintaining the gingival contours and allowed the patient to have fixed provisional at the day of the surgery. The authors highlighted the importance of an intact socket and a sufficient primary stability of the implant for the described surgical procedure.
ALVEOLAR RIDGE AUGMENTATION
STUDY BUCCAL FAT PAD-DERIVED STEM CELLS WITH ANORGANIC BOVINE BONE MINERAL SCAFFOLD FOR AUGMENTATION OF ATROPHIC POSTERIOR MANDIBLE: AN EXPLORATORY PROSPECTIVE CLINICAL STUDY.
Khojasteh A, Hosseinpour S, Rezai Rad M, Alikhasi M, Zadeh HH. Clin Implant Dent Relat Res. 2019 Apr;21(2):292-300.
https://www.ncbi.nlm.nih.gov/pubmed/30821120
This study aims to evaluate the efficacy of buccal fat pad-derived stem cells (BFPSCs) mixed with cerabone® in comparison to autologous bone for vertical and horizontal augmentation of the posterior mandible.
Methods:
14 patients with horizontal and vertical alveolar ridge deficiencies of less than 4 and 8 mm respectively were treated with cerabone® either preloaded with BFPSCs (group 1) or mixed with autologous bone chips (group 2). A titanium mesh was used to cover the grafts and to stabilize the augmented sites. The surface areas of newly formed bone were determined by quantitative CBCT analysis. Images were taken pre-operative and six months post-surgery.
Results:
– Total areas of newly formed bone were 5 ± 5.90 (group 1) and 166.75 ± 10.05 mm2 (group 2)
– Areas of new bone formation for vertical defects were 164.91 ± 3.74 (group 1) and 169.36 ± 12.09 mm2 (group 1)
– The area of new bone formation for horizontal deficiencies were 170.51 ± 4.54 mm2 (group 1) and 166.98 ± 9.36 mm2 (group 2)
– Differences between the two groups were not statistically significant
Conclusion:
The authors concluded that BFPSCs may be an alternative to autologous bone in alveolar ridge reconstruction as no differences in bone volume formation between the groups were found.
CASE SERIES ON HORIZONTAL GBR WITH CERABONE® AND JASON® MEMBRANE
Periosteal Envelope Flap as a Technique for Horizontal Bone Augmentation: A Case Series Study.
Arab S, Reza Arab H, Aghaloo M, Shiezadeh F, Tajik S, Moeintaghavi A. (2018). The Open Dentistry Journal. 12. 995-1003.
https://benthamopen.com/FULLTEXT/TODENTJ-12-995
This study aims to evaluate the efficacy of buccal fat pad-derived stem cells (BFPSCs) mixed with cerabone® in comparison to autologous bone for vertical and horizontal augmentation of the posterior mandible.
Methods:
14 patients with horizontal and vertical alveolar ridge deficiencies of less than 4 and 8 mm respectively were treated with cerabone® either preloaded with BFPSCs (group 1) or mixed with autologous bone chips (group 2). A titanium mesh was used to cover the grafts and to stabilize the augmented sites. The surface areas of newly formed bone were determined by quantitative CBCT analysis. Images were taken pre-operative and six months post-surgery.
Results:
– Total areas of newly formed bone were 5 ± 5.90 (group 1) and 166.75 ± 10.05 mm2 (group 2)
– Areas of new bone formation for vertical defects were 164.91 ± 3.74 (group 1) and 169.36 ± 12.09 mm2 (group 1)
– The area of new bone formation for horizontal deficiencies were 170.51 ± 4.54 mm2 (group 1) and 166.98 ± 9.36 mm2 (group 2)
– Differences between the two groups were not statistically significant
Conclusion:
The authors concluded that BFPSCs may be an alternative to autologous bone in alveolar ridge reconstruction as no differences in bone volume formation between the groups were found.
TREATMENT OF PERIODONTAL BONE DEFECTS
CASE REPORT GUIDED TISSUE REGENERATION IN SURGICAL ENDODONTIC TREATMENT: CASE REPORT AND LITERATURE REVIEW
Sidiropoulos, K., Roussou, K., Intzes, L., & Economides, N. (2019). Balkan Journal of Dental Medicine, 23(2), 102-107.
https://content.sciendo.com/abstract/journals/bjdm/23/2/article-p102.xml
This case report demonstrates the use of Guided Tissue Regeneration (GTR) for the treatment of a perio-endo lesion.
Methods:
Tooth 35 of a female patient was diagnosed with a pocket depth of 12 mm and grade two mobility. Radiographic analysis revealed an extended bone defect with involvement of the buccal plate and the presence of overextended filling material. Following root canal treatment, a periapical surgery using GTR was performed. After granulation tissue removal, cerabone® was applied, which was covered by a collagen membrane. The flap was closed and after one week, the sutures were removed.
Results:
An elimination of the periodontal pocket and a reduction of the mobility of the tooth was noted one year post-operative. Radiographic analysis revealed elimination of the periapical lesion. Two years post-surgery a reconstruction of the buccal plate was demonstrated by CBCT analysis. The patient remained asymptomatic over the whole observation period.
Conclusion:
The authors concluded that the endodontic-periodontal lesion could be efficiently treated by the described GTR procedure.
STUDY NONINCISED PAPILLAE SURGICAL APPROACH (NIPSA) IN PERIODONTAL REGENERATION: PRELIMINARY RESULTS OF A CASE SERIES.
Moreno Rodriguez JA, Caffesse RG. Int J Periodontics Restorative Dent. 2018;38(Suppl):s105-s111.
https://www.ncbi.nlm.nih.gov/pubmed/30118534
This case series aims to clinically evaluate a new surgical approach to treat periodontal intrabony defects in conjunction with cerabone® and Emdogain®. Surgically, the defects are accessed via the alveolar mucosa preserving the interdental tissues (Nonincised Papillae Surgical Approach, NIPSA).
Methods:
Ten patients diagnosed with periodontal intrabony defects with a mean probing pocket depth (PPD) of 9.6 ± 2.3 mm were treated with the Nonincised Surgical Approach (NIPSA) in conjunction with cerabone® and Emdogain®. PPD reduction, clinical attachment level gain (CAL), keratinized tissue width and recessions were recorded six to 18 months post-surgery.
Results:
Healing was uneventful in all cases. PPD decreased to 2.3 ± 0.5 mm and a CAL gain of 7.3 ± 2.4 mm was found. Gingival papilla height, keratinized tissue width and buccal gingival margin remained stable over time. All defects presented negative bleeding on probing.
Conclusions:
Deep isolated intrabony defects can be successfully treated using the Nonincised Surgical Approach (NIPSA) in conjunction with cerabone® and Emdogain®. NIPSA preserves the interdental papillae and marginal keratinized tissues avoiding post-operative soft tissue shrinkage.
DATABÁZE PUBLIKACÍ
LITERATURA
1 Tawil G, Tawil P, Khairallah A. Sinus Floor Elevation Using the Lateral Approach and Bone Window RepositioningI: Clinical and Radiographic Results in 102 Consecutively Treated Patients Followed from 1 to 5 Years. Int J Oral Maxillofac Implants. 2016 Jul-Aug;31(4):827-34.
2 Cardaropoli D, Tamagnone L, Roffredo A, De Maria A, Gaveglio L. Preservation of Peri-implant Soft Tissues Following Immediate Postextraction Implant Placement. Part II: Clinical Evaluation. Int J Periodontics Restorative Dent. 2019 Nov/Dec;39(6):789-797.
3 Kamadjaja DB, Sumarta NPM, Rizqiawan A. Stability of Tissue Augmented with Deproteinized Bovine Bone Mineral Particles Associated with Implant Placement in Anterior Maxilla. Case Rep Dent. 2019 Oct 27;2019:5431752.
4 Lorean A, Mazor Z, Barbu H, Mijiritsky E, Levin L. Nasal floor elevation combined with dental implant placement: a long-term report of up to 86 months. Int J Oral Maxillofac Implants. 2014 May-Jun;29(3):705-8.
5 Khojasteh A, Hassani A, Motamedian SR, Saadat S, Alikhasi M. Cortical Bone Augmentation Versus Nerve Lateralization for Treatment of Atrophic Posterior Mandible: A Retrospective Study and Review of Literature. Clin Implant Dent Relat Res. 2016 Apr;18(2):342-59.
6 Seidel P, Dingeldein E. cerabone® – Bovine Based Spongiosa Ceramic Seidel et al. Mat.-wiss. u. Werkstofftech. 2004
7 Khojasteh A, Motamedian SR, Rad MR, Shahriari MH, Nadjmi N. Polymeric vs hydroxyapatite-based scaffolds on dental pulp stem cell proliferation and differentiation. World J Stem Cells. 2015 Nov 26; 7(10): 1215–1221.